Brain Body Mind Lab
"It's not about seeing different things,
it's about seeing the same things differently."
- Marc Noël
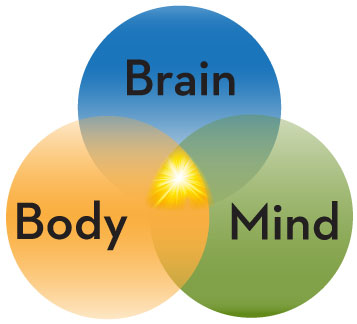
Investigating how MINDSET impacts healing and well-being by studying the synergy of Brain-Body-Mind.
MINDSET is the conscious and unconscious choices we make about the way we think and what we believe, our awareness and expectations, and our attitude and outlook. Here in the Brain Body Mind Lab, we are driven to discover innovative treatments incorporating how mindset works in synergy with Brain-Body-Mind to help recovery, healing, function, empowerment, self-image, and with that, quality of life.
We all experience challenges related to our health at some point in our lives which affects our bodies, brains and our minds.
Medical professionals have been successful at solving problems associated with acute disease. However, issues associated with chronic disease and chronic pain management have proven to be more challenging. Consequently, many patients receiving conventional care are additionally turning to complementary and integrative approaches.
As various complementary and integrative approaches gain wider acceptance, it is important to better understand how they work, and subsequently identify patients who would benefit most from complementary and integrative approaches used in conjunction with conventional care.
Examples of our areas of interest:
- The effect of cognitive multisensory rehabilitation (focused on body awareness and quality of movement) to improve sensory and motor recovery in people with stroke
- Develop outcome measures to assess body awareness and quality of movement of the upper limb in people with stroke
- Improve outcome measurements for body awareness and body image
- Investigate how Qigong practice mediates changes brain function and affects overall health in people with chronic diseases and chronic pain
- Identify how a change in mindset causes changes in brain function and affects overall health in people with chronic diseases.
"All revolutionary changes are unthinkable until they happen,
and then they are understood to be inevitable."
- Theodore Roszak
This is a new frontier in rehabilitation. If you would like to learn more or get involved in our journey of discovery, please click the appropriate link below.
2023
Zhang JJ, Van de Winckel A. Editorial: Insights in interventions for rehabilitation: 2023. Front Rehabil Sci. 2023 Nov 17;4:1326850. doi: 10.3389/fresc.2023.1326850. PMID: 38046522; PMCID: PMC10691531.
Van de Winckel A, Carpentier S, Deng W, Zhang L, Battaglino R, Morse L. Using remotely delivered Spring Forest Qigong™ to reduce neuropathic pain in adults with spinal cord injury: protocol of a quasi-experimental feasibility clinical trial. Pilot Feasibility Stud. 2023 Aug 22;9(1):145. doi: 10.1186/s40814-023-01374-3. PMID: 37608389; PMCID: PMC10464017.
Kimberley TJ, Prudente CN, Engineer ND, Dickie DA, Bisson TA, Van de Winckel A. Vagus Nerve Stimulation Paired With Mobility Training in Chronic Ischemic Stroke: A Case Report. Phys Ther. 2023 Dec 6;103(12):pzad097. doi: 10.1093/ptj/pzad097. PMID: 37669130; PMCID: PMC10748760.
Feng S, McDaniel S, Van de Winckel A. Finding functionality: Rasch analysis of the Functionality Appreciation Scale in community-dwelling adults in the US. Front Rehabil Sci. 2023 Oct 2;4:1222892. doi: 10.3389/fresc.2023.1222892. PMID: 37849959; PMCID: PMC10577199.
Van de Winckel A, Carpentier ST, Deng W, Zhang L, Philippus A, Monden KR, Battaglino R, Morse LR. Using remotely delivered Spring Forest Qigong™ to reduce neuropathic pain in adults with spinal cord injury: A non-randomized controlled trial. medRxiv [Preprint]. 2023 Feb 15:2023.02.11.23285793. doi: 10.1101/2023.02.11.23285793. PMID: 36824929; PMCID: PMC9949188.
Van de Winckel A, Zhang L, Hendrickson T, Lim KO, Mueller BA, Philippus A, Monden KR, Oh J, Huang Q, Ruen J, Konczak J, Evans R, Bronfort G. Identifying body awareness-related brain network changes after Spring Forest Qigong™ practice or P.Volve low-intensity exercise in adults with chronic low back pain: a feasibility Phase I Randomized Clinical Trial. medRxiv [Preprint]. 2023 Feb 14:2023.02.11.23285808. doi: 10.1101/2023.02.11.23285808. PMID: 36824785; PMCID: PMC9949220.
Van de Winckel A, Carpentier ST, Deng W, Bottale S, Zhang L, Hendrickson T, Linnman C, Lim KO, Mueller BA, Philippus A, Monden KR, Wudlick R, Battaglino R, Morse LR. Identifying Body Awareness-Related Brain Network Changes after Cognitive Multisensory Rehabilitation for Neuropathic Pain Relief in Adults with Spinal Cord Injury: Delayed Treatment arm Phase I Randomized Controlled Trial. medRxiv [Preprint]. 2023 Feb 10:2023.02.09.23285713. doi: 10.1101/2023.02.09.23285713. PMID: 36798345; PMCID: PMC9934787.
Deng W, Carpentier S, Blackwood J, Van de Winckel A. Rasch validation of the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS) in community-dwelling adults. BMC Psychol. 2023 Feb 17;11(1):48. doi: 10.1186/s40359-023-01058-w. PMID: 36803574; PMCID: PMC9936469.
Deng W, Carpentier S, Van de Winckel A. Physical body experiences questionnaire simplified for active aging (PBE-QAG): Rasch validation. PLoS One. 2023 Feb 10;18(2):e0280198. doi: 10.1371/journal.pone.0280198. PMID: 36763606; PMCID: PMC9916545.
Francisco GE, Engineer ND, Dawson J, Kimberley TJ, Cramer SC, Prudente CN, Pierce D, Tarver WB, Hinds RHA, Van de Winckel A, Yozbatiran N. Vagus Nerve Stimulation Paired With Upper-Limb Rehabilitation After Stroke: 2- and 3-Year Follow-up From the Pilot Study. Arch Phys Med Rehabil. 2023 Mar 30:S0003-9993(23)00147-8. doi: 10.1016/j.apmr.2023.02.012. PMID: 37001842.
Blackwood J, Carpentier S, Deng W, Van de Winckel A. Preliminary Rasch analysis of the multidimensional assessment of interoceptive awareness in adults with stroke. PLoS One. 2023 Jun 2;18(6):e0286657. doi: 10.1371/journal.pone.0286657. PMID: 37267348; PMCID: PMC10237650.
Van de Winckel A, Ottiger B, Veerbeek JM, Nyffeler T, Vanbellingen T. Rasch validation of a new scale to measure dependency in arm use in daily life: the Upper Limb Lucerne ICF-based Multidisciplinary Observation Scale. Front Neurol. 2023 Jul 10;14:1154322. doi: 10.3389/fneur.2023.1154322. PMID: 37492854; PMCID: PMC10364475.
2022
Hartman J, Sharp A, Van de Winckel A, Tetreault K, & Pechak C. (2022). Exploring the Characteristics of Doctor of Physical Therapy Students Intending to Work in Medically Underserved Areas. Journal of Health Care for the Poor and Underserved 33(3), 1368-1382. doi:10.1353/hpu.
Mallinson T, Kozlowski AJ, Johnston MV, Weaver J, Terhorst L, Grampurohit N, Juengst S, Ehrlich-Jones L, Heinemann AW, Melvin J, Sood P, Van de Winckel A. Rasch Reporting Guideline for Rehabilitation Research (RULER): the RULER Statement. Arch Phys Med Rehabil. 2022 Jul;103(7):1477-1486. doi: 10.1016/j.apmr.2022.03.013. Epub 2022 Apr 12. PMID: 35421395.
Van de Winckel A, Kozlowski AJ, Johnston MV, Weaver J, Grampurohit N, Terhorst L, Juengst S, Ehrlich-Jones L, Heinemann AW, Melvin J, Sood P, Mallinson T. Reporting Guideline for RULER: Rasch Reporting Guideline for Rehabilitation Research: Explanation and Elaboration. Arch Phys Med Rehabil. 2022 Jul;103(7):1487-1498. doi: 10.1016/j.apmr.2022.03.019. Epub 2022 Apr 15. PMID: 35436496.
Van de Winckel A, Carpentier S, Deng W, Bottale S, Hendrickson T, Zhang L, Wudlick R, Linnman C, Battaglino R, Morse L. Identifying body awareness-related brain network changes after cognitive multisensory rehabilitation for reduced neuropathic pain in adults with spinal cord injury: Protocol of the pilot clinical trial. TSCIR. 2022.
2021
Kim S, Van de Winckel A, Thompson KL, Heyn P. Book Chapter 78 Complementary and Integrative Medicine in Brain Injury Medicine, Principles and Practice, Third Edition, editors: Nathan D. Zasler MD; Douglas I. Katz MD; Ross D. Zafonte DO.
Van de Winckel A, Nawshin T, Byron C. Exploratory Study for Using the mobile Hudl App with Telehealth: A Randomized Controlled Trial Shows Positive Impact on Home Exercise Program Adherence in People with Chronic Diseases and in Financial Distress. JMIR Formative Research 2021;5(3):e22659. doi: 10.2196/22659.
Sharp A, Schmidt A, Casto C, Van de Winckel A. Lapses in Professional Behavior Identified by Students of Physical Therapy. JAH. 2021. J Allied Health 2021;50(2):e53-e57.
2020
Van de Winckel A, De Patre D, Rigoni M, Fiecas M, Hendrickson TJ, Larson M, Jagadeesan BD, Mueller BA, Elvendahl W, Streib C, Ikramuddin F, Lim KO. Exploratory study of how Cognitive Multisensory Rehabilitation restores parietal operculum connectivity and improves upper limb movements in chronic stroke. Sci Rep. 2020 Nov 20;10(1):20278. DOI: 10.1038/s41598-020-77272-y. PMID: 33219267.
Larson M, Chantigian DP, Asirvatham-Jeyaraj N, Van de Winckel A, Keller-Ross ML. Slow-Paced Breathing and Autonomic Function in People Post-stroke. Front Physiol. 2020 Oct 30;11:573325. doi: 10.3389/fphys.2020.573325. eCollection 2020. PMID: 33192570.
Dawson J, Engineer ND, Prudente CN, Pierce D, Francisco G, Yozbatiran N, Tarver B, Casavant R, Kline D, Cramer SC, Van de Winckel A, Kimberley TJ. Vagus Nerve Stimulation Paired with Upper Limb Rehabilitation after Stroke: One-year Follow-up. Neurorehab Neural Repair. 2020 Jul;34(7):609-615. DOI: 10.1177/1545968320924361.
2019
Van de Winckel A, Gauthier L. A revised Motor Activity Log following Rasch validation (Rasch-based MAL-18) and consensus methods in chronic stroke and multiple sclerosis. Neurorehabil Neural Repair 2019, 33(10):787–791.
Grampurohit N, Van de Winckel A, Ehrlich-Jones L. Measurement Characteristics and Clinical Utility of the ABILHAND-KIDS for children with neuromuscular conditions. Arch Phys Med Rehabil. 2019, 100(9):1795–1796.
Van de Winckel A, Ottiger B, Bohlhalter S, Nyffeler T, Vanbellingen T. Comprehensive ADL outcome measurement after stroke: Rasch validation of the Lucerne ICF-based Multidisciplinary Observation Scale (LIMOS). Arch Phys Med Rehabil. 2019, 100(12):2314-2323.
2018
Van de Winckel A, Carey JR, Bisson TA, Hauschildt E, Streib C, Durfee W. Safety and Feasibility of Transcranial Direct Current Stimulation via Telerehabilitation in People with Stroke. Arch Phys Med Rehabil. 2018, 99(10):e74.
Van de Winckel A, Carey JR, Bisson TA, Hauschildt EC, Durfee WK. Home-Based Transcranial Direct Current Stimulation plus Tracking Training Therapy in People with Stroke: An Open-Label Feasibility Study. J NeuroEng Rehab. 2018, 15:83. https://doi.org/10.1186/s12984-018-0427-2.
Van de Winckel A, Ehrlich-Jones L. Measurement Characteristics and Clinical Utility of the Motor Evaluation Scale for Upper Extremity in Stroke Patients. Arch Phys Med Rehabil. 2018, 99(12):2657-2658. https://doi.org/10.1016/j.apmr.2018.08.176.
Van de Winckel A, Jarrar M, Grampurohit N, Ehrlich-Jones L. Measurement Characteristics and Clinical Utility of the ABILHAND Among People With Rheumatoid Arthritis. Arch Phys Med Rehabil. 2018, 99(8):1693–1694. https://doi.org/10.1016/j.apmr.2018.04.006.
2017
Frost KL, Chen M, Cassidy JM, Snow L, Hodges JS, Van de Winckel A, Kimberley TJK, Carey JR. Paired Associative Stimulation to Suppress Contralesional Corticospinal Excitability in Three People with Stroke Using N-of-1 Crossover Design. J Neurol Transl Neurosci. 2017, 5(2): 1084.
Van de Winckel A, Tseng YT, Chantigian D, Lorant K, Zarandi Z, Buchannan J, Zeffiro TA, Larson M, Olson-Kellogg B, Konczak J, Keller-Ross M. Age-Related Decline of Wrist Position Sense and its Relationship to Specific Physical Training. Frontiers Hum Neurosci. 2017, 11:570. doi: 10.3389/fnhum.2017.00570.
Van de Winckel A, Tseng Y.T., Chantigian D,Lorant K, Zarandi Z, Buchanan J, Konczak J, Zeffiro T, Olson-Kellogg B, Larson M, Keller-Ross M. Mapping Age-Related Changes in Wrist Proprioception. Arch Phys Med Rehabil. 2017, 98(10):e80-e81.
De Patre D, Van de Winckel A*, Panté F, Rizzello C, Zernitz M, Mansour M, Zordan L, Zeffiro T, O’Connor EE, Bisson T, Lupi A, Perfetti C. A case report of visual and motor recovery after 8 months of "cognitive therapeutic exercises" in cortical blindness. JNPT. 2017, 41(3):164-172. doi: 10.1097/NPT.0000000000000189. *shared first author
2016
De Patre D, Van de Winckel A. Strategies for Scientific Research in Neurocognitive Rehabilitation Riabilitazione Neurocognitiva. 2016, (3):216-229.
Krewer K, Van de Winckel A, Elangovan N, Aman JE, Konczak J. Commentary on: "Assessing proprioception: A critical review of methods" by Han et al. (2015). JSHS. 2016, 5(1):91-92.
2013
Van de Winckel A, Verheyden G, Wenderoth N, Peeters R, Sunaert S, Van Hecke W, Perfetti C, De Cock P, Desloovere K, Eyssen M, Feys H. Does somatosensory discrimination activate different brain areas in children with unilateral cerebral palsy compared to typically developing children? An fMRI study. Res Dev Dis. 2013, 34(5):1710-1720. doi: 10.1016/j.ridd.2013.02.017.
Van de Winckel A, Klingels K, Bruyninckx F, Wenderoth N, Peeters R, Sunaert S, Van Hecke W, De Cock P, Eyssen M, De Weerdt W, Feys H. How does brain activation differ in children with unilateral cerebral palsy compared to typically developing children during active and passive movements, and tactile stimulation? An fMRI study. Res Dev Dis. 2013, 34(1):183–197. doi: 10.1016/j.ridd.2012.07.030.
2012
Van de Winckel A, Wenderoth N, Feys H, Sunaert S, Peeters R, Thijs V, Swinnen S, Perfetti C, De Weerdt W. Frontoparietal involvement in passively guided shape and length discrimination: A comparison between subcortical stroke patients and healthy controls. Exp Brain Res. 2012, 220(2):179-189. doi: 10.1007/s00221-012-3128-2.
Klingels K, Feys H, De Wit L, Jaspers E, Van de Winckel A, Verbeke G, De Cock P, Molenaers G. Arm and hand function in children with unilateral cerebral palsy: A one-year follow-up study. Eur J Paediatr Neurol. 2012, 16(3):257-265. doi: 10.1016/j.ejpn.2011.08.001.
Verhoeven J, Rommel N, Prodi E, Leemans A, Zink I, Vandewalle E, Noens I, Wagemans J, Steyaert J, Boets B, Van de Winckel A, Decock P, Sunaert S. Is there a common neuro-anatomical substrate of language deficit between Autism Spectrum Disorder and Specific Language Impairment? Cereb Cortex. 2012, 22(10):2263-2271. doi: 10.1093/cercor/bhr292.
2011
Vanbellingen T, Kersten B, Van de Winckel A, Bellion M, Baronti F, Müri R, Bohlhalter S. A new bedside test of gestures in stroke: The apraxia screen of TULIA (AST). J Neurol Neurosurg Psychiatry. 2011, 82(4):389-392. doi: 10.1136/jnnp.2010.213371.
2010
Klingels K, Jaspers E, Van de Winckel A, Huysmans A, Feys H. A systematic review of arm activity measures for children with hemiplegic cerebral palsy. Clin Rehabil. 2010, 24(10):887-900. doi: 10.1177/0269215510367994.
Vanbellingen T, Kersten B, Van Hemelrijk B, Van de Winckel A, Bertschi M, Müri R, De Weerdt W, Bohlhalter S. Comprehensive assessment of gesture production: a new test of upper limb apraxia (TULIA). Eur J Neurol. 2010, 17(1):59-66. doi: 10.1111/j.1468-1331.2009.02741.x.
2007
Van de Winckel A, Feys H, Lincoln N, De Weerdt W. Assessment of arm function in stroke patients: Rivermead Motor Assessment arm section revised with Rasch analysis. Clin Rehabil. 2007, 21(5):471-479.
Verheyden G, Nieuwboer A, Van de Winckel A, De Weerdt W. Clinical tools to measure trunk performance after stroke: a systematic review of the literature. Clin Rehabil. 2007, 21(5):387-394.
2006
Van de Winckel A, Feys H, van der Knaap S, Messerli R, Baronti F, Lehmann R, Van Hemelrijk B, Pante F, Perfetti C, De Weerdt W. Can quality of movement be measured? Rasch analysis and inter-rater reliability of the Motor Evaluation Scale for Upper Extremity in Stroke Patients (MESUPES). Clin Rehabil. 2006, 20(10):871-884.
Van de Winckel A. Commentary on "Physiotherapy assessment of knee proprioception following stroke" by Piriyaprasarth et al (2006). IJTR. 2006, 13(10):456.
2005
Van de Winckel A, Sunaert S, Wenderoth N, Peeters R, Van Hecke P, Feys H, Horemans E, Marchal G, Swinnen S, Perfetti C, De Weerdt W. Passive Somatosensory Discrimination Tasks in Healthy Volunteers: differential networks involved in familiar versus unfamiliar shape and length discrimination. NeuroImage. 2005, 26(2):441-453.
2004
Van de Winckel A, Feys H, De Weerdt W, Dom R. Cognitive and behavioral effects of music-based exercises in patients with dementia. Clin Rehabil. 2004, 18(3):253-260.
2001
De Weerdt W, Nuyens G, Feys H, Van Gronsveld P, Van de Winckel A, Nieuwboer A, Osaer J, Kiekens C. Group Physiotherapy improves time use by patients with stroke in rehabilitation. Aust J Physiother. 2001, 47(1):53-61.
2000
De Weerdt W, Selz B, Nuyens G, Staes F, Swinnen D, Van de Winckel A, Nieuwboer A, Lysens R, Feys H. Time use of stroke patients in an intensive rehabilitation unit: A comparison between a Belgian and a Swiss setting. Disabil Rehabil. 2000, 22(4):181-186.
Feys H, De Weerdt W, Nuyens G, Selz B, Van de Winckel A, Kiekens C. Predicting motor recovery of the upper limb following stroke rehabilitation: value of a clinical examination. Physiother Res Int. 2000, 5(1):1-18.
2024 Excellence in Complementary and Integrative Rehabilitation Medicine Research Award - Awarded by the Complementary Integrative Rehabilitation Medicine Networking Group Executive Committee of the American Congress of Rehabilitation Medicine (ACRM)
2021 Service Commendation American Congress of Rehabilitation Medicine for Task Force Co-Chair Measurement Interdisciplinary Special Interest Group Rasch Reporting Guidelines (ACRM)
Elite Reviewer for 2019 for the Archives of Physical Medicine and Rehabilitation
Training in Grantsmanship for Rehabilitation Research (TIGRR) Fellowship, 2019-2020 (Sponsored by NIH/NICHD)
APTA Early Career Award, 2016
Training in Grantsmanship for Rehabilitation Research (TIGRR) Fellowship, 2014
Funding: NIH (National Center for Complementary and Integrative Health, NCCIH)
Funding: Minnesota Spinal Cord Injury and TBI Grant Program 2022
Role: Principal Investigator
Funding: NIDILRR Department of Health and Human Services
Timeline: 9/1/2021-8/31/2025
Role: Co-Investigator
fMRI compatible robot
Clinical assessment batteries
Therapy material for cognitive multisensory rehabilitation (also known as "cognitive therapeutic exercises")
The MotionMonitor by Innovative Sports Training, Inc.
Center for Clinical Movement Science
Center for Magnetic Resonance Research
Center for Spirituality and Healing
Cognitive Multisensory Rehabilitation (Villa Miari, Vicenza, Italy)
Cognitive Multisensory Rehabilitation (Abruzzo, Italy)
Complementary, Alternative, or Integrative Health
Institute for Engineering in Medicine
National Center for Complementary and Integrative Health (NCCIH)
Director
Ann Van de Winckel, PhD, MSPT, PT
Principal Investigator
Contact
Email: avandewi@umn.edu
University of Minnesota
Division of Physical Therapy
420 Delaware Street SE
MMC 388
Minneapolis, MN 55455