U of M study looks to overcome the heterogeneity associated with treatment-resistant depression
For years, the M Physicians Interventional Psychiatry Clinic in St. Louis Park, MN, has been on the forefront of caring for patients who have treatment-resistant depression (TRD). TRD is diagnosed when patients fail at least two therapeutic treatment trials for their depression, according to Assistant Professor and psychologist Devin Hanson, PhD, LP, who is a member of the clinic’s patient care team.

Depression is considered both a major mental illness and a disability under the Americans with Disabilities Act. It is difficult to treat successfully. “Our current clinical impact when using traditional treatments is modest at best,” said Professor Ziad Nahas (pictured here), MD, MSCR, a renowned expert in treatment-resistant depression research. “We do not have treatments that work for everyone and struggle with the heterogeneity that depression presents.”
Treatment is evolving
The good news is that TRD treatment is evolving – and the U of M is at the forefront of that evolution. “My colleagues are investigating exciting new approaches,” said Hanson. “Sometimes, the treatments are brand new – on the very cutting edge – other times, it’s about fine-tuning treatments already approved by the Food and Drug Administration.”
One such cutting-edge study has Nahas collaborating with Damien Fair, PhD, of the Department of Pediatrics; David Darrow, MD, MPH; and Michael C. Park, MD, PhD, of the Neurosurgery Department; and Tay Netoff, PhD, in Bioengineering.
Building on previous work
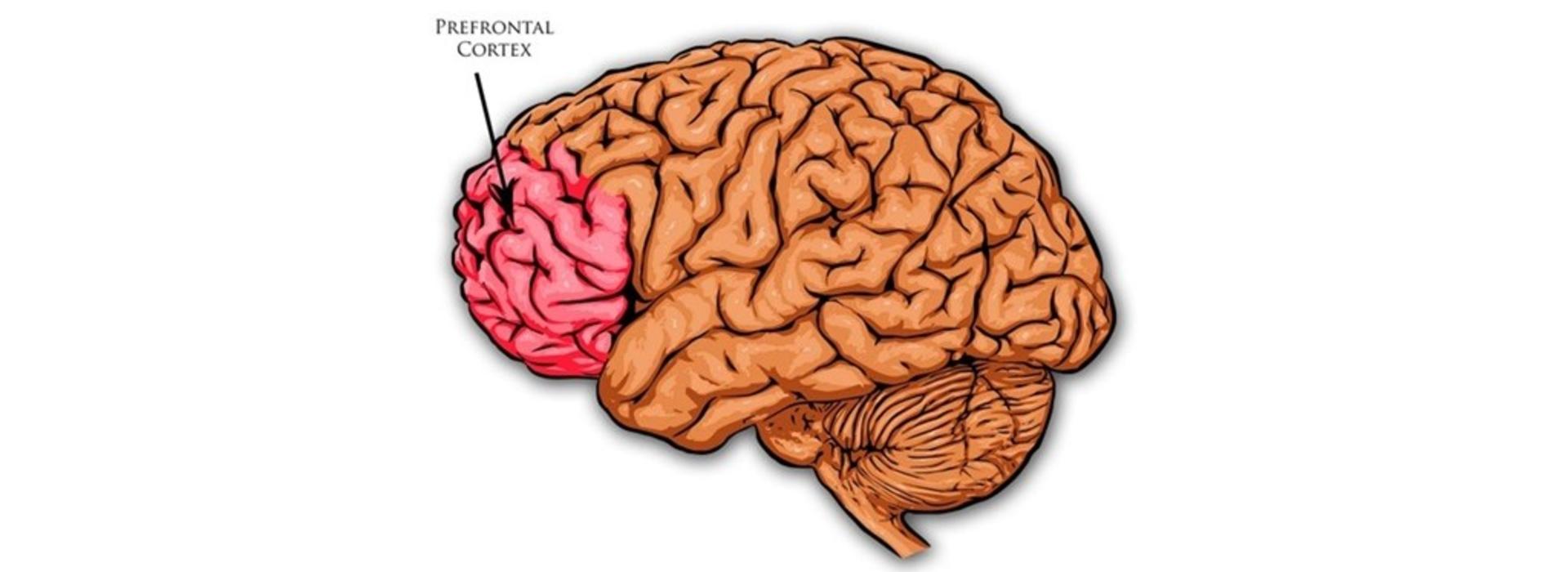
The researchers are building on a small TRD study (five participants) that Nahas conducted several years ago. It investigated the use of minimally invasive prefrontal cortical stimulation (PCS) to target specific areas of the brain’s surface critical in regulating mood with the implanted electrodes. The goal was to electrically reset underperforming circuits, with the aim of improving the patient’s depression. As a result, 60 percent of the study’s participants were in remission at 7 months and again at 5 years.
The research team has dubbed the new U of M study PCS2.0. “We’re taking advantage of additional technical achievements such as reliable individualized functional brain maps that help the team be more specific when tailoring stimulation targeting,” said Nahas. “We are also partnering with Bioengineering to use optimal mathematical models to home in on the correct stimulation settings and make the entire process more effective and efficient.”
Access to large-scale networks
This procedure, if it turns out to be effective, is not as invasive as deep brain stimulation, which requires passing materials through brain tissue. “Having access to large-scale networks on the surface of the brain is simpler, safer, and in some ways, easier,” said Nahas. He believes the procedure may also have the potential to treat other neurological conditions because of the nature of the surgical targeting.

Hanson (pictured here) was drawn to the team because they’re doing this kind of cutting-edge work in an interprofessional environment. “To treat patients – and do research – we benefit from the expertise of a team of providers such as psychiatrists, nurses, and social workers, as well as from colleagues in other departments,” he said. “I find it really gratifying.”
Nahas believes PCS2.0 has exciting potential because the researchers are taking precise brain images that help them understand what’s happening with patients on a case-by-case basis. “The imaging enables us to look at functional networks that may not be optimal in each participant’s brain,” he said. “We then target the stimulation to change the activity within these networks with the expectation that it will help improve that patient’s depression.” If successful, the team will have taken TRD treatment a giant step forward.
Keeping participants safe
There are a number of safeguards for the patients in this study. “To qualify, you undergo a comprehensive psychological, psychiatric, and medical evaluation,” said Nahas. “We present the candidates to our Data Safety and Monitoring Board, which is independent from the U. We also present the case to the deep brain surgery presurgical planning and ethical committee.”
Finally, when the team goes through the consent process with a potential participant, they administer a scale that assesses competency, and make sure that a patient advocate, such as a caregiver or family member, is present. “Our Institutional Review Board also monitors the consenting process to ensure that we don’t give study participants any false expectations,” said Nahas.
The study hopes to recruit 15 participants from an age range of 22 to 55 years. “That’s to minimize comorbidities that come with age,” said Nahas. One patient has already been implanted, the second is planned for January 2024. Currently, Medicare is covering the surgery and device costs incurred by participants. Going forward, this work is building the foundation for the team to secure a National Institute of Health BRAIN Initiative UH3 clinical trial study grant.