Program Overview
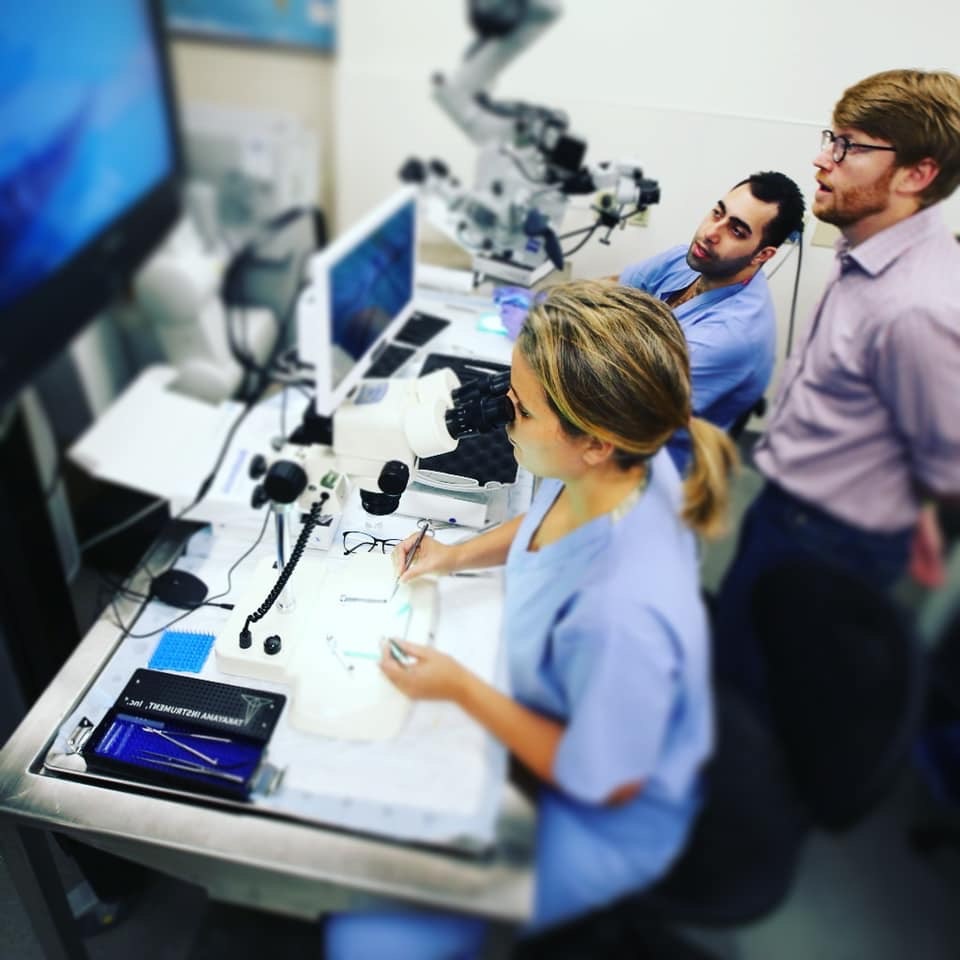
Blending tradition and innovation, we are a premiere, stable neurosurgery academic center focused on educational excellence, cutting-edge research, and skilled, compassionate patient care.
On average, we accept two new residents into the Neurosurgery Residency Program each year. Will one be you?
Welcome from the Director
We are proud of our long-standing tradition in graduating competent, skilled neurosurgeons. Our program was established in 1937 and has trained almost 150 neurosurgeons, including several who went on to become chairs of neurosurgery departments around the world. At the completion of training, we expect big things from you, either in your local community or in providing service to organized neurosurgery and medicine as a whole.

The Neurosurgery Residency Program at the University of Minnesota exposes you to all fields of neurosurgery in the full range of potential practice settings. We work hard to create an environment that fosters your growth in every aspect.
We create leaders
Our vision is to prepare you to be a leader in whatever practice setting you choose, be it private practice or academic neurosurgery. The training program is primarily based at the University of Minnesota; however, it includes rotations at Hennepin Healthcare, the University of Minnesota Masonic Children's Hospital and Minneapolis Veterans Affairs Medical Center. Each of these rotations gives you critical pieces of the training required to become certified by the American Board of Neurological Surgery.
Research key part of program
In addition, you are expected to spend 18 months in a dedicated research program, which ranges from enfolded fellowship training in endovascular neurosurgery to basic laboratory research.
Please let us know what we can do to help you decide to join us in this important endeavor.
Michael C. Park, MD, PhD
Associate Professor and Residency Program Director
MnDRIVE Neuromodulation Scholar
Patient Care
Residents must be able to provide patient care that is compassionate, appropriate and effective for treating health problems and promoting health.
Residents are expected to:
- Communicate effectively and demonstrate caring and respectful behaviors when interacting with patients and their families
- Gather essential and accurate information about their patients
- Make informed decisions about diagnostic and therapeutic interventions based on patient information and preferences, up-to-date scientific evidence, and clinical judgment
- Develop and carry out patient management plans
- Counsel and educate patients and their families
- Use information technology to support patient care decisions and patient education
- Perform competently all medical and invasive procedures considered essential for the practice area
- Provide health care services aimed at preventing health problems or maintaining health
- Work with health care professionals, including those from other disciplines, to provide patient-focused care.
Medical Knowledge
Residents must demonstrate knowledge about established and evolving biomedical, clinical, and cognate (for example, epidemiological and social-behavioral) sciences and applying this knowledge to patient care.
Residents are expected to:
- Demonstrate an investigatory and analytic thinking approach to clinical situations
- Know and apply basic and clinically supportive sciences that are appropriate to their discipline.
PRACTICE-BASED LEARNING AND IMPROVEMENT
Residents must be able to investigate, evaluate and improve their patient care practices and appraise and assimilate scientific evidence.
Residents are expected to:
- Analyze practice experience and perform practice-based improvement activities using a systematic methodology
- Locate, appraise and assimilate evidence from scientific studies related to their patients’ health problems
- Obtain and use information about their own population of patients and the larger population from which their patients are drawn
- Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information about diagnostic and therapeutic effectiveness
- Use information technology to manage information, access online medical information, and support their own education
- Facilitate the learning of students and other health care professionals.
INTERPERSONAL AND COMMUNICATION SKILLS
Residents must be able to demonstrate interpersonal and communication skills that result in effective information exchange and teaming with patients, their patients’ families, and professional associates.
Residents are expected to:
- Create and sustain a therapeutic and ethically sound relationship with patients
- Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning and writing skills
- Work effectively with others as a member or leader of a health care team or other professional group.
Professionalism
Residents must demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population.
Residents are expected to demonstrate:
- Respect, compassion and integrity
- Responsiveness to the needs of patients and society that supersedes self-interests
- Accountability to patients, society and the profession
- Commitment to excellence and ongoing professional development
- Commitment to ethical principles pertaining to providing or withholding clinical care, confidentiality of patient information, informed consent, and business practices
- Sensitivity and responsiveness to patients’ culture, age, gender, and disabilities.
Systems-based Practice
Residents must demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value.
Residents are expected to:
- Understand how their patient care and other professional practices affect other health care professionals, the health care organization, and the larger society and how these elements of the system affect their own practice
- Know how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources
- Practice cost-effective health care and resource allocation that does not compromise quality of care
- Advocate for quality patient care and help patients deal with system complexities
- Know how to partner with health care managers and health care providers to assess, coordinate and improve health care and know how these activities can affect system performance.
Program Outline
Neurosurgery residency training at the University of Minnesota is a six-year program following a one-year internship. The training is designed to give residents increasing clinical and surgical responsibility. Graduates prepare for an academic neurosurgical career, a high-quality practice in a private sector, or further training in a subspecialty fellowship.
Applications for Postgraduate Year 1 positions can be made through the National Resident Match Program.
The goal of PGY-1 is to learn the basics of evaluating and managing patient care in a clinical and surgical setting. Emphasis is on preoperative and postoperative management of the surgical patient, a multidisciplinary approach to the complicated patient, and emergency room evaluation. It includes:
• Neurosurgery - 5 months - University of Minnesota Medical Center
• Neuro ICU - 1 month - University of Minnesota Medical Center
• Neurology - 2 months - Hennepin Healthcare
• Critical Care - 4 months - University of Minnesota Medical Center; 2 months - Hennepin Healthcare.
The goal of PGY-2 is to begin learning the basics of neurosurgery. This includes obtaining the presenting neurologic history, performing the examination, and formulating an appropriate management plan. The resident will learn and become proficient in the basic neurosurgical operations and will assist in more complex procedures.
• 12 months – University of Minnesota Medical Center
• 6 months – Hennepin Healthcare
• 6 months – University of Minnesota Medical Center
• 6 months – Elective Rotation/Research
• 6 months – Neuropathology/Pediatrics – University of Minnesota Medical Center/University of Minnesota Masonic Children's Hospital
• 12 months – Elective Rotation/Research
• 6 months – Senior Resident, University of Minnesota Medical Center
• 6 months – Chief Resident, Veterans Affairs Medical Center
• 6 months – Chief Resident, University of Minnesota Medical Center
• 6 months – Chief Resident, Hennepin Healthcare
Program Requirements
As part of the training in neurosurgery at the University of Minnesota, residents are required to develop competencies in six general areas as stipulated by the Accreditation Council for Graduate Medical Education (ACGME).